- Cleanings & Oral Exams, to keep your teeth and gums healthy, and catch early signs of dental disease
- Cosmetic Bonding, to repair small chips or cracks
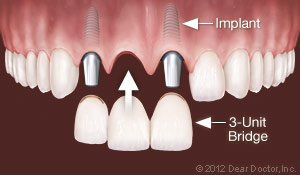
- Crowns & Bridgework, to replace large amounts of lost tooth structure and/or missing teeth
- Dental Implants, for the longest-lasting tooth replacement available today
- Extractions, to remove unhealthy teeth that cannot be saved
- Fillings, to restore decayed teeth
- Inlays & Onlays, to fill teeth with larger cavities
- Invisalign Clear Aligners, for highly discreet orthodontic treatment
- Oral Cancer Screenings, to detect a dangerous disease that can be cured if caught early
- Orthodontic Treatment, to move teeth into the right position
- Porcelain Veneers, for repairing larger chips and cracks, and reshaping teeth
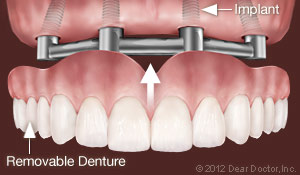
- Removable Dentures, to help you smile again
- Root Canal Treatment, to rescue diseased teeth
- Sealants, to help prevent cavities
- Teeth Whitening, to brighten a faded or discolored smile
- TMD Treatment, for pain in the jaw area that can interfere with biting and chewing
- Tooth-Colored Fillings, for a completely natural, healthy look
- Tooth Decay Prevention, so you keep your natural teeth as long as possible
Orthodontics
What a difference straight teeth can make! A great-looking smile can boost your self-confidence and have a positive impact on social and professional opportunities. Orthodontic treatment is the original smile makeover tool — and you will be happy to know that you're never too old to take advantage of it. But it isn't all about looks: Properly aligned teeth help you to bite, chew and even speak more effectively. They are also easier to clean, which helps keep your mouth free of tooth decay and gum disease.
The amazing thing about orthodontics is that it harnesses the body's natural ability to remodel its own tissue. With the application of light, constant force, orthodontic appliances gently reshape bone and move teeth into better positions. Some examples of these appliances are traditional metal braces, inconspicuous clear or tooth-colored braces, and clear aligners, a relatively new option for adults and teens.
Bite Problems and How to Fix Them
Orthodontic treatment can resolve a number of bite problems, which often become evident by around age 7. These include underbite, crossbite or excessive overbite, where upper and lower teeth don't close in the proper position; open bite, where a space remains between top and bottom teeth when the jaws are closed; and crowding or excessive spacing, where teeth are spaced too close together or too far apart.
To correct bite problems, teeth need to be moved — but doing that isn't as hard as you might think! Teeth aren't fixed rigidly in their supporting bone; instead, they're held in place by a hammock-like structure called the periodontal ligament, which is very responsive to forces placed on the teeth. Orthodontic appliances move teeth by careful application of light, constant pressure. This force can be applied via metal wires that run through small brackets attached to the teeth (braces), or via the semi-rigid plastic of clear aligners.
Orthodontics is for Children — and Adults
Having orthodontic treatment in childhood is ideal in order to take advantage of a youngster's natural growth processes to help move the teeth into proper alignment. Like the rest of the body, the teeth and jaws are now changing rapidly. So at this time it's possible (for example) to create more room for teeth in a crowded mouth by using a “palatal expander” to rapidly widen the upper jaw. This phase of growth modification can shorten overall treatment time and ensure the best result if additional orthodontic appliances are needed.
But remember, healthy teeth can be moved at any age, so you've never “missed the boat” for orthodontic treatment. In fact, about one in five of today's orthodontic patients is an adult. Several new technological developments — including tooth-colored ceramic braces, clear aligners and invisible lingual braces — have made orthodontic appliances less evident, and enhanced the treatment experience for grown-ups. Before treatment, adults are carefully examined for signs of periodontal (gum) disease, which will be brought under control before treatment begins.
To correct bite problems, teeth need to be moved — but doing that isn't as hard as you might think! Teeth aren't fixed rigidly in their supporting bone; instead, they're held in place by a hammock-like structure called the periodontal ligament, which is very responsive to forces placed on the teeth. Orthodontic appliances move teeth by careful application of light, constant pressure. This force can be applied via metal wires that run through small brackets attached to the teeth (braces), or via the semi-rigid plastic of clear aligners.

When you imagine someone wearing braces, you probably picture small metal brackets bonded to the front of the teeth, with a thin wire running through them. This time-tested style remains very popular — but it's no longer the only option. Clear braces use brackets made of ceramic or plastic which, except for the slim archwire, are hardly visible. Lingual braces are just like traditional metal braces — except they're bonded to the back of your teeth (the tongue side) so that no one can see them.
Removable clear aligners are an alternative to fixed orthodontic appliances. They consist of a series of clear plastic “trays” that fit over your teeth exactly; each one moves your teeth a little bit, until they are in the proper position. Whether fixed or removable, each type of appliance may have advantages or disadvantages in particular situations. After a complete examination, the best treatment options for you will be discussed.
Retention & Post Orthodontic Care
Once your orthodontic treatment is completed, it's extremely important to wear a retainer as directed. That's because teeth naturally tend to drift back to their original locations — which is the last thing you want after you've gone to the trouble of straightening them! Wearing a retainer holds your teeth in their new position long enough for new bone and ligament to re-form around them, and helps keep your gorgeous new smile looking good for a lifetime.
Implant Dentistry
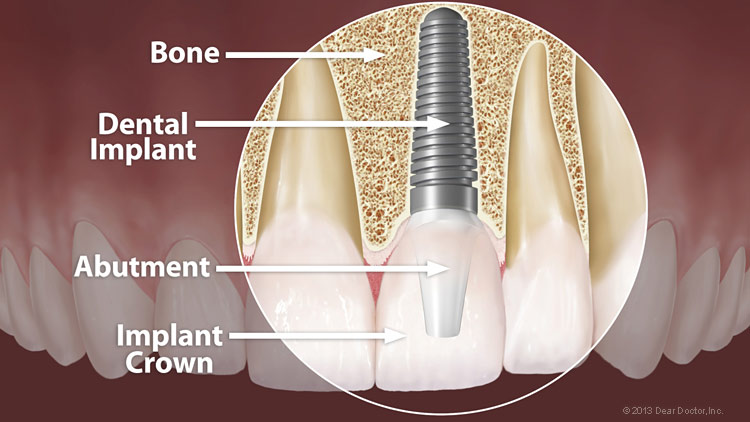
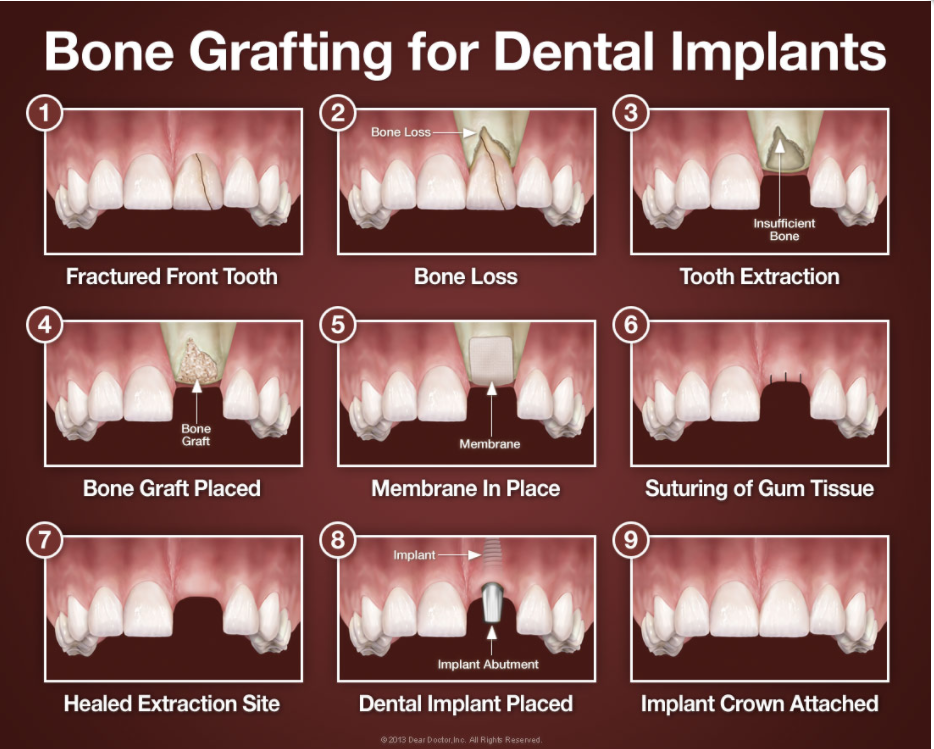
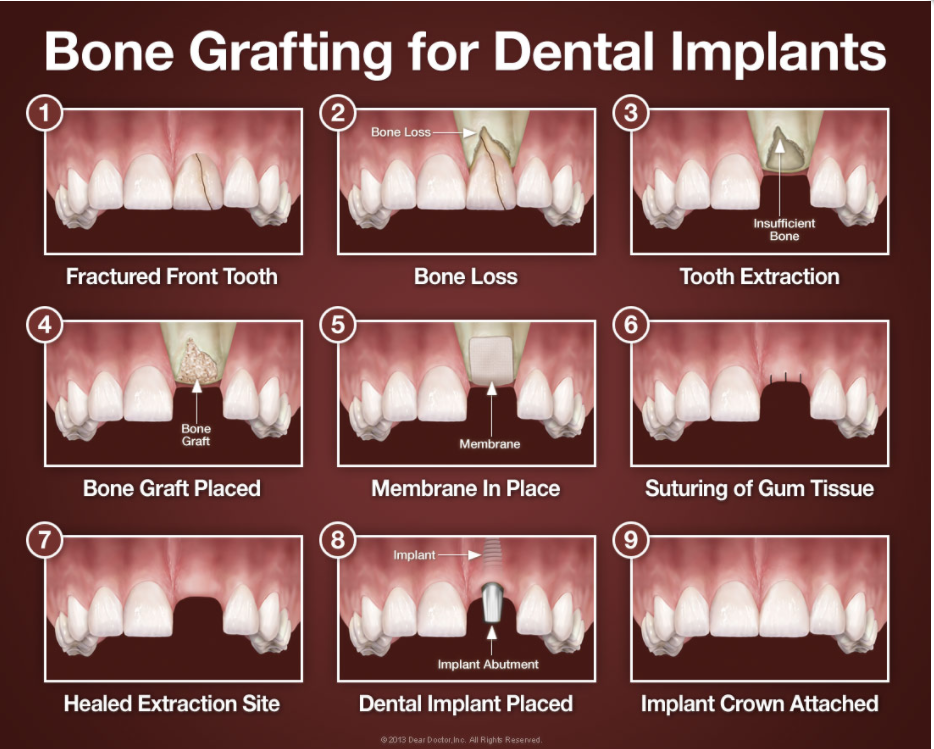
Implant Dentistry Search Of all the ways modern dentistry has to replace missing teeth, dental implants are by far the best. There is no tooth-replacement option that will give you a longer-lasting result. Implants also help preserve tooth-supporting bone that naturally deteriorates when a tooth is lost. Loss of bone is one of the major hidden consequences of losing teeth.
Dental Implant.
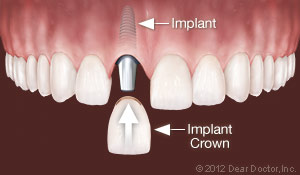
A dental implant most often takes the form of a small, screw-shaped titanium post that replaces the root-part of a missing tooth. The surgical procedure used to place an implant is actually quite minor and routine, requiring only local anesthesia in most cases. After a healing period, the implant is topped with a lifelike crown custom-made to match your existing natural teeth. Implants have a documented success rate of over 95%, which is significantly higher than any other tooth-replacement option.
How Implants Work
During a minor surgical procedure, your dental implant is inserted directly into the jawbone in the space vacated by the missing tooth. It will then be left to heal for a period of months before the final crown is attached. During this healing period, the implant actually fuses to the bone surrounding it.
Tooth Replacement Options Using Dental Implants
Implants can replace missing teeth in a variety of ways. They can be used to:
Tooth Replacement Options Using Dental Implants
Replace One Tooth — When you have one tooth missing, a single implant is inserted into the bone to replace the root part of that tooth; a crown then goes on top to simulate an actual tooth. This treatment choice has the highest success rate, making it the best long-term investment for replacing a single missing tooth. Even if the initial cost is slightly higher than other options, it is the most cost-effective solution over time. An implant will never decay or need root canal treatment, and feels just like the tooth that was there.
Replace Multiple Teeth — When you have more than one tooth missing, implants provide an ideal replacement mechanism. You don't even need one implant for every missing tooth. Instead, implant teeth can act as supports for fixed bridgework. For example, if you are missing three teeth in a row, we can place two implants, one on either side of the gap, and a crown in between that has no implant underneath. That way, you won't need to use any of your remaining natural teeth as bridge supports, which could weaken them and make them more susceptible to decay.
Replace All Teeth Permanently — Implants can support an entire arch of upper or lower replacement teeth that are fixed into the mouth and are never removed. Sometimes the new teeth can be supported by as few as 4 implants. It's comparable to the structure of a table, which only needs 4 legs to hold it up. In cases where jawbone density and volume have deteriorated, 5 or 6 implants might be needed to support a row of 10 to 12 teeth. Dental implant replacement teeth protect your jawbone, won't slip, and should last a lifetime.

Support Removable Dentures — Implants can even make removable dentures more comfortable, effective and healthier to wear. Traditional dentures rest on the gums and put pressure on the underlying bone. This accelerates bone loss so that the jaw shrinks and the dentures slip, particularly on the bottom. But today dentists can attach a removable denture onto implants, transferring that pressure into the bone structure rather than the bone surface. This prevents the dentures from slipping while you eat and speak, and preserves the bone directly beneath them.
Implant Care and Maintenance
There are only two ways an implant can lose attachment to the bone and fail once it has successfully fused: poor oral hygiene or excessive biting forces. Poor oral hygiene and/or a lack of regular cleanings can lead to a destructive bacterial infection called peri-implantitis. Flossing and brushing your teeth on a daily basis, along with regular professional cleanings, can prevent this. Excessive biting forces can come from either a habit of clenching or grinding your teeth, or an insufficient number of implants to handle the forces generated by your bite. You should receive the correct number of implants so this does not happen. And if you have a habit of grinding or clenching your teeth, a nightguard will be recommended to protect your implants. After all, implants are a long-term investment in your smile, your health and your well-being, so it's best to protect your investment.
Sedation Dentistry

Winslow Dental offers Sedation dentistry.
Dr. Gardner and staff are highly trained to offer sedation dentistry for the comfort and safety of patients.
Sedation dentistry is great for patients with:
- Fear or anxiety of dentist
- Hate shots and needles
- Traumatic past experiences
- Gag reflex
- Long appointments
Same Day Crowns



Only Specially trained dental practices with the right equipment and technology can place same day crowns. Patients love that we don't have to use the old gooey impressions and wait for a couple weeks for a lab to make and mail a crown. Winslow Dental can fix your tooth with a crown and have you on your way in no time. A same day crown is a fast and precise way to fix your teeth, that looks great, works great, and lasts. There are many advantages to same day crowns. Your teeth are digitally scanned and the crown is custom designed to fit and look great. Once the crown is placed, it is permanent and you are able to brush, floss and care for it just like the rest of your teeth.
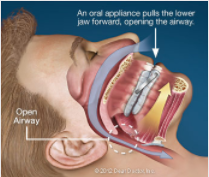
Sleep Apnea
Do you:
Snore, or ever been told you snore?
Experience daytime fatigue?
Wake up with morning headaches?
Diagnosed with sleep apnea, or wear a CPAP?
Winslow Dental can help you. There is an option for you called Oral Appliance Therapy, and it is covered by most insurances.
Unsure if you have Sleep Apnea?
Take our Sleep Risk Assesment
Cosmetic Contouring
Sometimes little defects in teeth can attract more than their fair share of attention. The eye often seems drawn to the tiny chip in a front tooth; the slight mismatch in tooth size among adjacent teeth; the extra-pointy canine. If you find yourself staring at these subtle yet distracting features in your own smile, help is available — often with a minimally invasive, relatively inexpensive procedure known as tooth contouring (reshaping).
Tooth contouring involves removing a tiny amount of tooth enamel with a drill to sculpt a more pleasing shape and make the tooth fit in better with its neighbors. The tooth is then polished for a smooth finish. The procedure is most often used on the upper front incisors and canines, which are your most visible teeth.
Cosmetic problems that can be corrected with tooth contouring include: small chips, uneven tooth length, slight overlaps, and tooth edges that are too flattened or pointy. It can even be used to correct minor bite problems from teeth touching unevenly during contact. Conversely, your teeth should not be reshaped if any bite imbalances could result from it. In that case, one of several other highly effective cosmetic dental procedures would be recommended. Tooth contouring can also be used to give teeth a more feminine or masculine shape, simply by rounding or squaring the edges.
What to Expect
The first step in the contouring procedure is to examine your teeth and diagnose how the reshaping will accomplish your goal of smile enhancement or correct a bite problem if you have one. This will ensure that the teeth being reshaped will not only look better but also will be healthy. Sometimes a reshaping of the root surfaces is required to protect you from gum disease. In that case, an x-ray may be necessary to isolate and protect the sensitive inner tissue (the pulp). However, most often tooth contouring only involves the removal of a bit of enamel — the hard outer covering of the tooth. Because enamel is not living and contains no nerves, you will likely not need even a local anesthetic.
You will probably feel some vibration as your tooth is gently sculpted, and then polished smooth. Reshaping one tooth usually takes less than half an hour — and the results will be obvious as soon as you look in the mirror! Sometimes reshaped teeth can be a little sensitive to hot or cold after the procedure, but this should last no more than a day or two.
Tooth contouring can be combined with whitening for a dramatically younger-looking smile. It's also often used in conjunction with cosmetic bonding or dental veneers — both of which can be used to reshape teeth with larger imperfections.
Cosmetic Dentistry
The practice of dentistry encompasses an amazing array of services and procedures, all with a common goal: to help you to preserve your natural teeth as long as possible, ensure your oral health, and keep you looking and feeling great throughout life. There's so much that can be done these days to improve the appearance of a person's smile — at any age. From powerful, professional whitening treatments to amazingly realistic porcelain veneers to state-of-the-art dental implants, there's a wide range of exciting possibilities.
The first step in any smile makeover is a thorough dental examination to make sure that your cosmetic problems really are just that, and not a sign of underlying dental disease. Once your health has been established, your smile can be cosmetically enhanced in a variety of ways.
Cosmetic & General Dentistry Procedures
Modern dentistry offers a wide range of services to make sure your teeth stay healthy, function well and look great. These procedures include:
Bridges
Crowns can also be used to create a lifelike replacement for a missing tooth. This is done with bridgework, which spans the space of the missing tooth and requires at least three crowns. Two of those crowns will be placed over healthy teeth on either side of the missing tooth; these healthy teeth are referred to as abutment teeth. The two crowned abutment teeth become supports for a third crown placed in between them; that third crown is referred to as a pontic. If more than one tooth is missing, more crowns will be needed to bridge the gap in between the abutment teeth.
The number of abutment teeth necessary to replace missing teeth is influenced by the number of missing teeth, the size and length of the abutment tooth roots, the amount of bone support each abutment tooth has, as well as where in the mouth the missing tooth is located. For example, if you have three missing teeth, four abutment teeth may be necessary, thereby creating a seven-tooth bridge. Engineering and designing of the bridge requires an understanding of how to replace teeth, as well as the biology of the supporting gum and bone tissue.
Caring for Your Crowns & Bridgework
Crowns and bridgework require the same conscientious care as your natural teeth. Be sure to brush and floss between all of your teeth — restored and natural — every day to reduce the buildup of dental plaque. When you have crowns, it is even more important to maintain your regular schedule of cleanings at the dental office. Avoid using your teeth as tools (to open packages, for example). If you have a grinding habit, wearing a nightguard would be a good idea to protect your teeth and your investment.
Dentures

Full or partial tooth loss, if left untreated, doesn't just affect a person's self-image — it can also increase the risk of developing nutritional problems and other systemic health disorders. Fortunately, there's a reliable and time-tested method for treating this condition: full or partial dentures.
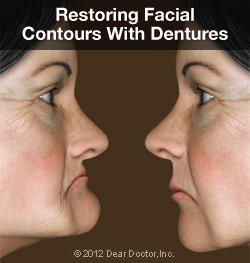
Dentures are just one option for replacing missing teeth; some of the others include fixed bridgework and dental implants. Each method has its particular pluses and minuses, which should be carefully considered. There are also several varieties of dentures available to address specific issues, from partial dentures to implant-supported overdentures. The best option for you will depend on your individual situation.
How Do Removable Dentures Work?
Full or partial dentures consist of a gum-colored base made of plastic resin, which fits over the remaining alveolar (bone) ridge that formerly held the teeth. The prosthetic teeth projecting from the base are designed to look and function just like your natural teeth. Dentures are held in place primarily by the suctioning effect of their close fit against the alveolar ridges — that's why it's so important that they are fitted properly. The upper denture also gets extra support from the large surface area of the roof of the mouth (palate), which generally makes it extremely stable.
At first, wearing dentures may require some getting used to in terms of talking and eating, as the dentures become “balanced” in the space formerly occupied by the teeth. But over time, the muscles, nerves and ligaments of the mouth learn to work in new ways, which allows these functions to occur normally. Dentures also help support the facial skeleton and the soft tissues of the lips and cheeks, which can help create a more youthful appearance.
Types of Full Dentures
Immediate Dentures: These are usually a temporary means of helping you transition to successful denture wearing. Because of the muscular readjustment required, as well as the natural shrinkage of gums, the dentures which are placed immediately after tooth extraction won't fit as well as permanent dentures made when the healing is complete. They do, however, provide you with new teeth right away, and give you time to adjust.

Conventional Full Dentures: After a period of time, permanent dentures that conform to your mouth with near-perfect accuracy can be fabricated. These are carefully crafted to look as much like your own natural teeth as possible, and are able to function properly in your mouth for a long time.
Implant-Supported Overdentures: To increase the stability of a lower or upper denture, it's possible for it to be securely anchored using two or more dental implants. The upper jaw requires more implants (generally three or more) than the lower jaw due to a lesser bone density. Many people find this option offers a great balance of comfort, functionality and value.
Types of Partial Dentures
Transitional Partial Dentures: These relatively inexpensive removable plastic dentures serve as a temporary tooth replacement and space maintainer as you wait for your mouth to heal from tooth extraction, for example. Once the healing process is complete, dental implants can be placed.
Removable Partial Dentures (RPDs): Usually made of cast vitallium, these well-constructed, metal-based removable partial dentures are much lighter and less obtrusive than those made of plastic. They are a little more expensive than plastic dentures but will fit better. They are, however, much less expensive than implants or fixed bridgework.
How Dentures Are Made and Fitted
Making quality dentures is a blend of science and art. First, an accurate impression (mold) is made of the alveolar ridges on the top and bottom of your mouth. The base of the denture is made from this mold in a dental laboratory. Working together, the dentist and lab technician choose from among many different sizes and shapes of prosthetic teeth to re-create a natural-looking smile. When everyone is satisfied with the result, the temporary dentures are made in permanent form.
To enable normal speech and eating, it's crucial to balance your bite. This means that the upper and lower dentures come together and properly stabilize each other. The form and function of the dentures are carefully checked to ensure that they are working and fitting properly.

What to Expect After You Get Dentures
If you've recently lost your teeth and received an immediate denture, it's normal to find some tissue shrinkage and bone loss occurring. Therefore, in several months you may find that your immediate dentures no longer fit well. You will have two choices at this point: You can have your immediate (temporary) dentures re-lined. This means that material is added under the denture's base to better conform to the new contours of your alveolar ridge. A better option is to move to a set of conventional full dentures, which will last longer and fit better. With proper care, dentures offer a functional, aesthetic and economical solution to the problem of tooth loss.
Root Canal Treatment Is Your Friend
Root canal treatment — also called endodontics (“endo” – inside, “dont” – tooth) — is a set of specialized procedures designed to treat problems of the soft pulp (nerve) tissue inside the tooth. While some mistakenly think of it as an unusually painful treatment, in most cases the procedure is no more uncomfortable than getting a filling. It's actually one of the most effective ways of relieving some kinds of tooth pain.
A root canal procedure becomes necessary when infection or inflammation develops in the pulp tissue of the tooth. Pulp tissue consists of blood vessels, connective tissue and nerve cells — which explains why a problem here may cause you to feel intense pain. In time, the pain may go away... at least temporarily. Without treatment, however, the infection won't. It can lead to a dental abscess, and may even contribute to systemic problems in other parts of the body.

Root Canal Treatment
We've all heard the gag: “I'd rather have a root canal...” This comedy line, comparing the procedure to something truly undesirable, may be funny — but putting off needed endodontic treatment is no joke. The idea that a root canal procedure invariably comes with complications and pain is a shopworn myth. It's certainly true that infection or inflammation in the tooth's pulp can be excruciatingly painful. But you should remember that having a root canal results in eliminating this acute pain and is not the cause of the pain.
Need another reason not to delay root canal treatment? How about this: A natural tooth that's saved via root canal treatment and restoration helps you avoid the problems that commonly occur when teeth must be removed. These include unwanted tooth migration or shifting, which can lead to difficulties in chewing; the need for bridgework or dental implants, which may be costly and complicated; and even the eventual loss of bone structure from the area of the missing tooth.
Causes of Root Canal Problems
Root canal problems stem from infection and inflammation of the tooth's pulp tissue. One potential cause of infection is deep tooth decay. Untreated dental cavities eventually allow bacteria to work their way down to the center of the tooth, where they may infect the pulp tissue. Another path by which bacteria may come into contact with pulp is via chipped or cracked teeth. Any opening in the protective enamel coating has the potential to allow bacteria access to the tooth's pulp.
Trauma to the tooth — the kind that might result from a sports injury or automobile accident, for example — is also a major cause of pulp tissue damage. In this case, it's essential to seek treatment immediately, both to try and save the tooth, and to prevent future problems.
In some cases, extensive dental work itself may cause damage to the pulp tissue that will need to be treated via a root canal. Having multiple fillings or restorations on the same tooth increases the chances of this type of injury. Occasionally, common procedures like crown preparation or orthodontics may eventually lead to root canal problems.

What to Expect During Root Canal Therapy
If an examination shows that you do need root canal therapy, don't worry — it's one of the most routine and effective procedures in the arsenal of dental treatments and can often be accomplished in just one visit.
The root canal process generally begins the same way as a filling does, and with no greater discomfort: an anesthetic is administered to numb the tooth and the surrounding area. For many patients, the worst is already over.
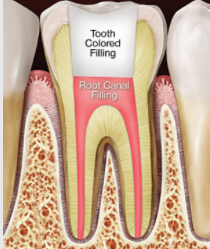
Next, a small opening is made in the surface of the affected tooth to give access to the pulp chamber and root canals. Tiny instruments are used, sometimes with the aid of a microscope, to remove the dead and dying pulp tissue from inside these narrow passageways. The chamber and empty canals are then cleaned, disinfected, and prepared to receive a filling of inert, biocompatible material. Finally, adhesive cement is used to seal the opening in the tooth, preventing future infection.
Following root canal treatment, your tooth may feel some sensitivity or tenderness for a few days. Over-the-counter pain relievers like ibuprofen are generally effective in relieving discomfort, but prescription medications may also be given if needed. During this period, it may help to avoid biting hard on the affected tooth. All of these symptoms, however, should be temporary.
To further protect the tooth and restore it to full function, it's usually necessary to have a crown or other restoration placed on it. Restorations can take many forms, from traditional gold crowns to tooth replicas made of high-tech tooth-colored material. In any case, you will have made an investment in preserving your dental health for years to come.
Signs and Symptoms of Root Canal Problems
How do you know when you need a root canal? Sometimes, it's painfully obvious. If you feel constant and severe pain and pressure in your mouth, or noticeable swelling and extreme sensitivity in your gums, then it's clear you need an evaluation and treatment right away. Another telltale symptom of pulp tissue damage is sharp pain when you bite down on food. Lingering pain after eating hot or cold foods is also an indication of potential trouble. If you notice any of these symptoms, you need to have an examination as soon as possible.
Periodontal Therapy
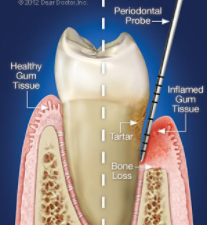
It is not a given that we must lose teeth as we age. If we maintain good oral hygiene and have regular professional cleanings and oral examinations, chances are we can keep our natural teeth for life. That involves not only caring for the teeth themselves, but also the structures that surround them: the gums and tooth-supporting bone. Gum disease, which is a bacterial infection, threatens these supporting tissues. That is why dental professionals are always on the lookout for early signs that patients may not notice. When signs of trouble become apparent, periodontal therapy may be suggested.
Periodontal therapy can take various forms, but the goal is always to restore diseased tissues to health. Gum (periodontal) disease can spread from the gums to the bone that supports the teeth, and may even cause tooth loss in the most severe cases. There are very effective therapies to combat this, ranging from scalings (deep cleanings) that remove plaque and calculus (tartar) from beneath the gum line, to surgical repair of lost gum and bone tissue.
Periodontal Therapy Procedures
Periodontal therapy includes both surgical and non-surgical techniques to restore health to the tissues that support the teeth (gums and bone) and prevent tooth loss. They include:
- Scaling and Root Planing. These deep-cleaning techniques are the best starting point to control gum disease. Plaque and calculus (tartar) are removed from beneath the gum tissues, using hand scalers and/or ultrasonic instruments.
- Gum Grafting. Sometimes it’s necessary to replace areas of lost gum tissue so that tooth roots are adequately protected. This can be accomplished by taking healthy gum tissue from one area of the mouth and moving it to where it is needed, or by using laboratory-processed donor tissue.
- Periodontal Plastic Surgery. When used to describe surgery, the word “plastic” refers to any reshaping procedure that creates a more pleasing appearance of the gum tissues.
- Periodontal Laser Treatment. Removing diseased gum tissue with lasers can offer significant advantages over conventional surgery, such as less discomfort and gum shrinkage.
- Crown Lengthening Surgery. This is a surgical procedure in which tooth structure that is covered by gum and bone tissue may need to be exposed either for cosmetic reasons (too make the teeth look longer and the smile less gummy) or to aid in securing a new dental crown.
- Dental Implants. Today’s preferred method of tooth replacement is a titanium dental implant, which is placed beneath the gum line and into the jawbone during a minor surgical procedure. The implant is then attached to a realistic-looking dental crown that is visible above the gum line and indistinguishable from a natural tooth.
Your Role in Periodontal Health
Dental plaque is the main cause of periodontal disease, so it's essential to remove it every day with effective brushing and flossing. This doesn't mean scrubbing, which can actually cause your gums to recede. Proper techniques can be demonstrated for you, if you have any questions.
Of course, there are some areas of the mouth that a toothbrush and floss just can't reach, which is why it's so important to have regular professional cleanings at the dental office. Your regular dental exam is also a time when early signs of gum disease can be detected — before they become apparent even to you.
Eating a nutritious diet low in sugar, and staying away from tobacco in all forms, will also increase your periodontal health — and your chances of keeping your teeth for life.
Maxillofacial Surgery

When you were a youngster, did you ever get a black eye, chip a tooth or bruise your cheek? If so, you may have experienced a case (let's hope, a mild one!) of facial trauma. In many situations, however, facial trauma can be severe. Among its major causes are auto accidents, sports injuries, work-related mishaps, falls, and acts of violence. When serious facial injury occurs, it's important that you receive immediate and comprehensive care. That's why oral and maxillofacial surgeons are on call at most emergency and trauma centers.
Facial trauma in general involves injuries to the soft- or hard-tissue structures of the face, mouth or jaws — including the teeth, the bones of the jaws and face, and the tissue of the skin and gums. It can also involve treatment of particular specialized regions, such as the area around the eyes, the salivary glands or facial nerves. Because facial injuries can affect not only a person's ability to carry on basic life functions (eating, vision, etc) but also his or her appearance, there is often a strong emotional component to treatment as well as a physical one. But after completing an extensive training program, oral and maxillofacial surgeons are capable of handling the full scope of facial injuries.
Treatments for Facial Injury
Some facial traumas are relatively minor. A common one occurs when a tooth is loosened or knocked out (avulsed). Many times, if treated immediately, the tooth can be successfully re-implanted in the jaw. If that isn't possible, placing a dental implant is often the most effective way to replace a missing tooth.
Another type of relatively common but more serious injury may involve a fracture of the facial bones, including the cheekbones, upper or lower jawbones, or the eye sockets. In principle, its treatment is essentially the same as that used for a broken arm: place the bones back in their proper position, and immobilize them. But since it isn't possible to put a cast on the face, different immobilization techniques are used. One method involves wiring the upper and lower jaws together to let them heal in the correct alignment; alternatively, plates and screws may be used to permanently reattach the bones.
Severe facial trauma is often a critical condition, since over 60% of these patients also have serious injuries in other parts of the body. In fact, many of the standard techniques used in trauma centers were developed by oral and maxillofacial surgeons during the wars in Korea, Vietnam, and the Middle East. Restoring breathing, controlling bleeding and checking for neurological damage are top priorities. After that, as much of the reconstructive surgery as possible is accomplished in one operation.

Preventing Facial Trauma
What's the best treatment for facial trauma? Prevention. Always wearing seat belts, using proper helmets and protective gear when playing sports, and staying out of dangerous situations (like driving while impaired, tired or distracted) can go a long way toward keeping you safe. If you're engaging in athletic activities that carry any risk of facial injury, wear a properly fitted mouthguard — this small piece of protective equipment can save you a lot of potential harm.
But if you (or someone you care for) require a trip to the emergency room for a facial injury, be sure to ask for a consultation with an oral and maxillofacial surgeon, so that you get the best care and the most favorable outcome.
Sealants

The most likely location for a cavity to develop in your child's mouth is on the chewing surfaces of the back teeth. Run your tongue over this area in your mouth, and you will feel the reason why: These surfaces are not smooth, as other areas of your teeth are. Instead, they are filled with tiny grooves referred to as “pits and fissures,” which trap bacteria and food particles. The bristles on a toothbrush can't always reach all the way into these dark, moist little crevices. This creates the perfect conditions for tooth decay.
What's more, a child's newly erupted permanent teeth are not as resistant to decay as adult teeth are. The hard enamel coating that protects the teeth changes as it ages to become stronger. Fluoride, which is found in toothpaste and some drinking water — and in treatments provided at the dental office — can strengthen enamel, but, again, it's hard to get fluoride into those pits and fissures on a regular basis. Fortunately, there is a good solution to this problem: dental sealants.
Dental sealants are invisible plastic resin coatings that smooth out the chewing surfaces of the back teeth, making them resistant to decay. A sealed tooth is far less likely to develop a cavity, require more expensive dental treatment later on, or, most importantly, cause your child pain.
Sealants
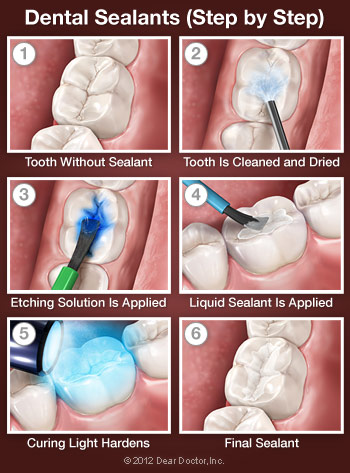
How Sealants Are Placed
You can think of a sealant as a mini plastic filling, though please reassure your child that it doesn't “count” as having a cavity filled. Because tooth enamel does not contain any nerves, placing a sealant is painless and does not routinely require numbing shots. First, the tooth or teeth to be sealed are examined, and if any minimal decay is found, it will be gently removed. The tooth will then be cleaned and dried. Then a solution that will slightly roughen or “etch” the surface is applied, to make the sealing material adhere better. The tooth is then rinsed and dried again. The sealant is then painted on the tooth in liquid form and hardens in about a minute, sometimes with the help of a special curing light. That's all there is to it!
A note about BPA: A 2012 study that received wide press coverage raised concerns that trace amounts of the chemical bisphenol-A (BPA) found in some (but not all) dental resins might contribute to behavioral problems in children. The study authors noted that while they had found an association, they had not actually proven that BPA in dental sealants causes these problems. In fact, BPA is far more prevalent in food and beverage packaging than in dental restorative materials. The American Academy of Pediatric Dentistry and the American Dental Association have since reaffirmed their support for the use of sealants.
Taking Care of Sealants
Sealed teeth require the same conscientious dental hygiene as unsealed teeth. Your child should continue to brush and floss his or her teeth daily and have regular professional cleanings. Checking for wear and tear on the sealants is important, though they should last for up to 10 years. During this time, your child will benefit from a preventive treatment proven to reduce decay by more than 70 percent.
Veneers

What makes a smile beautiful? That's a complex question, but some qualities of a lovely smile are immediately identifiable: good tooth color, shape and alignment are a few of the most important ones. If your teeth could use improvement in any of these categories, porcelain veneers could be just what you're looking for.
You may already know that a veneer is a thin covering over another surface. In dentistry, a veneer is a wafer-thin layer of super-strong porcelain that convincingly substitutes for natural tooth enamel. When bonded to your teeth, veneers can create a natural-looking, beautiful new surface. That's because dental porcelain, like natural tooth enamel, is translucent and tough. But it doesn't stain like tooth enamel does.
Recent years have brought remarkable advances in dental porcelain technology. These days, veneers can be made so thin that they can sometimes be bonded directly onto your existing tooth surface. In other cases, a very thin layer of tooth enamel — as thin as the veneer itself — needs to be removed to fit the new porcelain surface and make it look as lifelike as possible. Either way, the results are sure to make you smile.
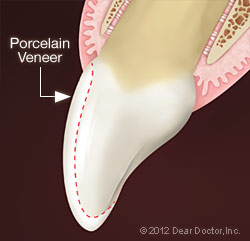
Versatility of Porcelain Veneers
Veneers can be used to improve any of the following characteristics of your teeth:
Color — Teeth can become stained by the foods and drinks we like, from smoking, and even normal aging. Veneers are available in numerous shades, from the most natural to the brightest Hollywood white.
Size & Shape — Teeth can become worn down from grinding habits, or may not have the shape or size you want to begin with. For example, some people consider rounder teeth more feminine and squarer teeth more masculine. Veneers can be shaped and sized in whichever way is most flattering to your face.
Alignment & Spacing — Veneers can be used to close small gaps between teeth or make slight corrections in alignment while improving tooth color and shape.

Limitations of Porcelain Veneers
There are some situations in which veneers would be inappropriate. For example, if you have significantly misaligned teeth or a large gap, orthodontics might be a more appropriate solution than veneers. And if you have lost a lot of tooth structure from decay or trauma (or a particularly severe grinding habit), it might be better to restore your teeth with porcelain crowns that cover the entire tooth.
Creating a New Smile with Porcelain Veneers
The first step in creating a new smile with porcelain veneers is to communicate exactly what you don't like about your smile as it is now. It's a great idea to bring in pictures of smiles you do like, as a starting point for discussion. It's possible to see how veneers would look on your teeth in one of several ways. A model of your teeth can be created over which wax “veneers” can be placed; sometimes acrylic (plastic) or tooth-colored filling material can be placed directly onto your teeth to demonstrate the effect veneers would have on them.
Once the plan has been agreed upon, your teeth will be prepared by removing a small amount of enamel, if this step is necessary. Molds of your teeth will be taken and used by a skilled dental laboratory to create your veneers, and you will receive a temporary set of veneers to wear during the few weeks it will take to create your permanent veneers. When the veneers come back from the lab, they will be cemented onto your teeth.
Caring for Your Veneers
Porcelain Veneers
Search
What makes a smile beautiful? That's a complex question, but some qualities of a lovely smile are immediately identifiable: good tooth color, shape and alignment are a few of the most important ones. If your teeth could use improvement in any of these categories, porcelain veneers could be just what you're looking for.
Porcelain veneer.You may already know that a veneer is a thin covering over another surface. In dentistry, a veneer is a wafer-thin layer of super-strong porcelain that convincingly substitutes for natural tooth enamel. When bonded to your teeth, veneers can create a natural-looking, beautiful new surface. That's because dental porcelain, like natural tooth enamel, is translucent and tough. But it doesn't stain like tooth enamel does.
Recent years have brought remarkable advances in dental porcelain technology. These days, veneers can be made so thin that they can sometimes be bonded directly onto your existing tooth surface. In other cases, a very thin layer of tooth enamel — as thin as the veneer itself — needs to be removed to fit the new porcelain surface and make it look as lifelike as possible. Either way, the results are sure to make you smile.
Versatility of Porcelain Veneers
Veneers can be used to improve any of the following characteristics of your teeth:
Porcelain veneers - before and after.
Color — Teeth can become stained by the foods and drinks we like, from smoking, and even normal aging. Veneers are available in numerous shades, from the most natural to the brightest Hollywood white.
Size & Shape — Teeth can become worn down from grinding habits, or may not have the shape or size you want to begin with. For example, some people consider rounder teeth more feminine and squarer teeth more masculine. Veneers can be shaped and sized in whichever way is most flattering to your face.
Alignment & Spacing — Veneers can be used to close small gaps between teeth or make slight corrections in alignment while improving tooth color and shape.
Limitations of Porcelain Veneers
There are some situations in which veneers would be inappropriate. For example, if you have significantly misaligned teeth or a large gap, orthodontics might be a more appropriate solution than veneers. And if you have lost a lot of tooth structure from decay or trauma (or a particularly severe grinding habit), it might be better to restore your teeth with porcelain crowns that cover the entire tooth.
Creating a New Smile with Porcelain Veneers
The first step in creating a new smile with porcelain veneers is to communicate exactly what you don't like about your smile as it is now. It's a great idea to bring in pictures of smiles you do like, as a starting point for discussion. It's possible to see how veneers would look on your teeth in one of several ways. A model of your teeth can be created over which wax “veneers” can be placed; sometimes acrylic (plastic) or tooth-colored filling material can be placed directly onto your teeth to demonstrate the effect veneers would have on them.
Once the plan has been agreed upon, your teeth will be prepared by removing a small amount of enamel, if this step is necessary. Molds of your teeth will be taken and used by a skilled dental laboratory to create your veneers, and you will receive a temporary set of veneers to wear during the few weeks it will take to create your permanent veneers. When the veneers come back from the lab, they will be cemented onto your teeth.
Caring for Your Veneers
Just like the teeth nature gave you, teeth restored with veneers need gentle brushing and flossing every day. This will remove dental plaque and ensure good gum tissue health around the veneers. Regular checkups at the dental office will remain as important as always to your oral and general health. And keep in mind that as tough as veneers are, they may not be able to withstand forces that come from using your teeth as tools (to open packages, for example) or biting into very hard foods like candy apples — which isn't good for your natural teeth, either! And if you grind or clench your teeth at night, you might be advised to get a custom-made nightguard to protect your veneers — and your investment.
Whitening
It's hard to imagine anything more appealing than a sparkling, white smile. Yet our teeth rarely stay as white as we'd like them to without a little help. Fortunately, that help is available at the dental office.
Teeth whitening done in a professional dental setting is a safe, effective way to brighten your smile. It's also perhaps the most economical cosmetic dental procedure. Depending on the whitening method you choose, results can be dramatic: in-office whitening, for example, can lighten teeth three to eight shades in a single hour.
Professionally supervised whitening will work faster, and protect sensitive gums and tooth-root surfaces better, than over-the-counter whitening products. Having an oral exam before you begin any whitening process is an important first step to make sure your tooth discoloration is not the result of a dental condition in need of treatment. Also, please be aware that it can be risky to have whitening solutions applied to your teeth by untrained personnel in shopping malls. If you have any questions about which whitening method would be best for you, talk to us first.
Professional Whitening Methods
Professional whitening makes use of high-concentration bleaching gels that are not available over the counter.

In-Office Whitening — This technique offers the fastest results with the most powerful whitening solutions available. First, your gums and tooth-root surfaces will be covered with a protective barrier to ensure your safety. A thin plastic device known as a retractor will hold your lips and cheeks away from your teeth as a professional-strength hydrogen peroxide gel is applied. The gel will be left on for about an hour. When it is removed, the results will be obvious immediately.
Take-Home Whitening — This is another effective way to whiten your teeth, though you will play a greater role in ensuring the best possible results and several weeks may be needed to achieve your desired level of whiteness. First, a mold of your teeth will be taken and then two thin, flexible plastic mouth trays will be custom-made for you — one for the top teeth and one for the bottom. You will fill the trays with whitening gel and then position the trays over your teeth. The trays are left in usually for about an hour at a time.
Caring for Your Whitened Smile
There are lots of things you can do to make sure your whitening results last as long as possible, and this will vary from person to person (six months to two years or even longer). First of all, please maintain your usual, conscientious routine of brushing and flossing every day, and keep up with your regular schedule of professional cleanings at the dental office. Avoid foods and beverages that stain, including red wine, tea and coffee. If you smoke, use your newly whitened teeth as an impetus to quit — a good idea in any event! A minor touch-up every so often, either at home or at the dental office, can keep your smile bright and beautiful for years.
Excessive or Uneven Gums
There are many elements that make up an ideal smile; bright, healthy-looking teeth immediately come to mind. But the gum tissue that surrounds and supports those teeth also plays a big role in how appealing your smile will look.
Cosmetic Gum Problems
Cosmetic Gum Surgery
Search
Cosmetic gum surgery.There are many elements that make up an ideal smile; bright, healthy-looking teeth immediately come to mind. But the gum tissue that surrounds and supports those teeth also plays a big role in how appealing your smile will look.
There are various cosmetic issues involving gum (gingival) tissue. For example, your smile may look “gummy” — meaning you seem to display too much gum tissue when you smile, or your teeth appear too short. Sometimes it's the opposite problem — your teeth appear too long because your gum tissue has receded (pulled back), exposing tooth-root surfaces that were covered at one time. Or, you may have an uneven gum line, meaning gum tissue covers some of your teeth more than others. All of these cosmetic gum problems can be successfully treated with cosmetic procedures performed in the dental office.
Cosmetic Gum Problems
Excess Tissue. A gummy smile can be caused by excessive gum tissue covering more enamel surface of a tooth's crown (upper portion) than normal. If that is the case, a procedure known as “crown lengthening” can be performed, in which gum tissue (and sometimes a small amount of bone tissue) is removed to expose more tooth surface.
Receding Gums. Sometimes your gums can shrink down (recede), exposing a portion of your tooth roots. This causes a cosmetic problem because root surfaces, which have no enamel covering, tend to appear more yellow than the crowns of your teeth. Also, exposed roots can be more sensitive to cold or touch, and can be at greater risk of decay. There are various gum-grafting procedures that can cover exposed roots, all of which involve moving gingival (gum) tissue from one site in the mouth to another. For example, roots can be covered with tissue from the roof of your mouth, which is of the same type; or adjacent (nearby) tissue can be moved over to cover an exposed root. Sometimes laboratory-processed tissue from another donor can even be used. All of these options can be discussed with you in more detail.
Uneven Gum Line. If you have an uneven gum line where some teeth are covered by more tissue than others, it is often possible to recontour (reshape) the tissue for a very pleasing effect. This can be done conventionally with a surgical scalpel or with newer dental laser technology. The advantage of a laser is that it seals the tissue as it sculpts it, making the procedure more comfortable and requiring a shorter healing time.
What to Expect
All cosmetic gum surgery can be performed at the dental office — and it usually requires only a local anesthetic (numbing shot). In fact, for laser surgery you may need only a topical anesthetic applied in gel form. If you would like a deeper level of relaxation, you can have oral or possibly even an IV sedative; but if this is required, you will need a ride home. Laser surgery leaves no open wounds and causes minimal, if any, discomfort, though the anatomy of the area may preclude laser use. An examination is required to determine whether conventional or laser treatment is in your best interests.
Grafts may take longer to heal, particularly if tissue is taken from the roof of your mouth. If that's the case, you will have two sites that need to heal: the donor site from which the tissue was taken, and the recipient site where the tissue was attached. Both of these sites will require stitches, usually of the dissolving type. You will need to eat a softer diet and avoid chewing on that side of your mouth for a few days. Though full healing may take a few weeks, you will be able to resume your normal activities the very next day. Whichever kind of cosmetic gum surgery you may need, the procedures are routine and predictable — and they can do wonders for your smile!
Extractions

The main goal of dentistry is to preserve your natural teeth and keep them healthy for as long as possible. There are times, however, when it is in your best interest (or your child's) to have a tooth extracted (removed). This could be the case for a variety of reasons. Perhaps you have a tooth that has been severely damaged by trauma or decay; or an impacted wisdom tooth that may cause trouble for you later on. Maybe your teenager will soon undergo orthodontic treatment and has insignificant space for his adult teeth, referred to as crowding. Or your younger child has a baby tooth that's stubbornly adhering, even though it's past time for it to go.
Whatever the reason, tooth extraction is more often than not a very routine procedure. How straightforward this minor surgery is will depend on where the tooth to be extracted is located in the mouth, and what its roots are like. For example, a front tooth with a single straight root is easier to remove than a molar with multiple roots. This is especially true when that molar is a wisdom tooth that is impacted, meaning it is below the surface surrounded by gum tissue and bone. Often, a wisdom tooth is blocked from fully erupting (growing in) by other teeth in its path.
Still, tooth extraction is nothing to be feared when done by an experienced hand. Keep in mind that a tooth is not rigidly fixed in its surrounding bone, though that's how some may picture it. In fact, it is attached to the bone via a network of fibers that form what's known as the periodontal ligament. By carefully manipulating the tooth, these fibers can be detached and the tooth freed without much trouble
Reasons for Extracting a Tooth
As mentioned above, there can be a variety of reasons for extracting a tooth. Be sure to ask questions about the pros and cons of any dental treatment, including extraction.
Trauma or Disease
In both of these situations, there are several ways to try and save the tooth. The damaged tooth might need a full-coverage crown, a root canal treatment, or both. But sometimes even these methods are not enough to keep the tooth functioning well and looking good; it might be better to remove the tooth and replace it with a strong and lifelike dental implant.
Orthodontic Treatment
Teeth are sometimes extracted when there are too many of them for the size of the dental arches (jaws), a situation known as crowding. After an adequate amount of space is opened up through the extraction of one or more teeth, the remaining teeth can be aligned properly. The teeth most frequently removed for orthodontic reasons are the first premolars, which are right next to the eyeteeth (canines).
Impacted Wisdom Teeth
Early removal of impacted wisdom teeth can prevent damage to neighboring healthy teeth, bone, gum tissue, even nerves and blood vessels. If an impacted wisdom tooth is in a bad position, it's best to remove it before its roots are fully formed.
Baby Teeth
If a baby tooth is out of position or not lost in the right sequence, the permanent tooth underneath it might not erupt normally. In this case, removing the baby tooth could prevent a need for orthodontic treatment later on.


The Process of Extracting a Tooth
The first step in any extraction is a radiographic (x-ray) examination to assess the position of the tooth roots and the condition of the surrounding bone. This will allow any possible complications to be anticipated. A thorough medical and drug history is taken, to ensure that you are healthy enough to undergo the procedure, and your options for anesthesia will be discussed.
Tooth extraction is usually carried out with local anesthesia, which will numb the teeth to be removed, and the surrounding bone and gum tissues. Additional sedatives might also be used, including oral sedatives (taken in pill form), nitrous oxide (which is inhaled) and/or conscious sedation, which is given intravenously (into a vein). The latter is usually required for more complicated (or multiple) tooth extractions. By the time the sedation medication has worn off, you won't even be aware that the surgery was done.
As your tooth is being removed, steps are taken to ensure the bone that surrounds it isn't damaged. Sometimes, in the process of removing a tooth, a small amount of lab-processed bone-grafting material is placed into the socket to help preserve the bone volume there. This is particularly important when the extraction is going to be followed at some point by the placement of a dental implant, which needs to fuse to existing bone, or orthodontics, which gently moves teeth through bone.
What to Expect After Tooth Extraction
mmediately after your tooth is extracted, the socket will be covered with sterile gauze; gentle pressure will be applied for 10-20 minutes to control any bleeding. Small sutures (stitches) might also be used for this purpose. It's normal to experience some mild to moderate post-operative discomfort and/or swelling. Taking non-steroidal, anti-inflammatory drugs such as ibuprofen and/or aspirin the day of surgery should control most symptoms. Antibiotics may also be prescribed to ensure infection-free healing. Using ice packs on the outside of your jaw, and eating softer foods until you feel more comfortable can also be helpful. Within a few days, all should be back to normal.
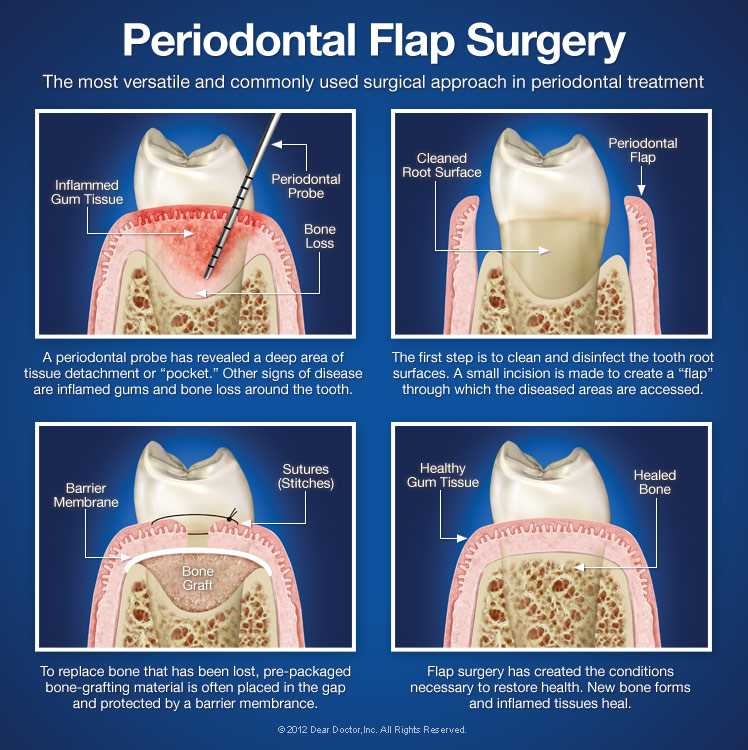
Flap Surgery

When advanced gum disease (periodontitis) develops, your teeth are in danger: At this stage, the ligaments and bone tissue that surround them are being destroyed, and you could even begin losing teeth! If the disease can't be controlled by non-surgical treatments like cleaning and scaling, then periodontal flap surgery may be your best treatment option.
Flap surgery is today's leading method for treating and repairing periodontal pockets. What are these “pockets?” They are areas below the gum line where gum tissue has detached from the teeth, resulting in an uncleansable space where harmful bacteria can proliferate. These bacteria cause inflammation of the tissues, resulting in sensitivity, bleeding, and pain. Left untreated, they can cause a host of problems including gum disease, loss of the tooth-supporting bone structure, and possibly even systemic (whole-body) problems.
When periodontal pockets develop, the first step in treating them is usually via cleaning and scaling (also referred to as root debridement) with a manual or ultrasonic instrument. If this isn't effective, then periodontal surgery is considered. Flap surgery isn't a cure for periodontal disease — but it helps create an environment that makes it easier to maintain your periodontal health. And even if you're prone to gum disease, proper professional treatment and regular care at home can help keep your teeth healthy for as long as possible.
The Goals of Flap Surgery
One major objective of flap surgery is to eliminate or reduce the pocket itself. To access it, a flap-like incision is made in the gum tissue. This allows diseased tissue to be removed from inside the pocket, and provides access to the teeth's root surfaces for a thorough cleaning, which helps to eliminate harmful plaque and calculus (tartar). Afterward, the “flap” is closed, sealing the area. This begins the healing process, which takes place rapidly.
Another goal is the regeneration of periodontal ligament and bone tissue which may have been lost to the disease. A variety of techniques may be used to accomplish this, including high-tech methods of bone grafting and chemicals referred to as growth factors. These approaches help restore the gums to their normal form and function, and promote the healthy and secure anchoring of teeth.
The Flap Surgery Procedure
Flap surgery is typically done under local anesthesia, sometimes accompanied by oral anti-anxiety medications; alternatively, it may be performed under intravenous conscious sedation. After anesthesia has taken effect, a small incision is made to separate the gums from the teeth. The outer gum tissue is gently folded back to give access to the roots and the supporting ligament and bone tissue.
Next, the inflamed gum tissue can be removed, and the tooth roots can be cleaned; if needed, the area may also be treated with antibiotics or other medications. Bone defects can be repaired with grafting material, and proper regeneration of the periodontal ligament can be encouraged by physical (barrier membranes) and chemical (growth factors) methods. Finally, the incision is closed and the procedure is completed.
Performed by an experienced hand, state-of-the-art flap surgery has an excellent track record and offers well-established benefits. It's often the treatment of choice for relieving periodontal disease and helping to maintain your oral health — and preserve your teeth.
Grafts
Muscle Pain — This can be felt in the cheeks (masseter muscles) and temples (temporalis muscles), where the two big pairs of jaw-closing muscles are located. If you feel soreness and stiffness upon waking up in the morning, it's often related to habits such as clenching and/or grinding the teeth at night. If you have this type of nocturnal habit, a custom-made nightguard should be very helpful in decreasing the force applied to your teeth, which will in turn allow your muscles to relax and relieve pressure on your jaw joints. Other self-care remedies are discussed below (please see Relieving the Pain).
Joint Pain — Pain that's actually coming from one or both jaw joints technically would be described as arthritis (“arth” – joint; “itis” – inflammation) of the TMJ. Radiographs (x-ray pictures) show that some people have arthritic-looking TMJs but no symptoms of pain or dysfunction; others have significant symptoms of pain and dysfunction but their joints look normal on radiographs. There is no cure for arthritis anywhere in the body, but medication can sometimes help relieve arthritic symptoms.
Relieving the Pain
Once you have been examined, a strategy for treating your condition and managing your pain can be developed. Sometimes a temporary change to a softer diet can reduce stress on the muscles and joints. Ice and/or moist heat can help relieve soreness and inflammation. Muscles in spasm can also be helped with gentle stretching exercises. Non-steroidal anti-inflammatory medications and muscle relaxants can also provide relief.
Other Treatment Options
Severe TMD cases may require more complex forms of treatment, which might include orthodontics, dental restorations like bridgework, or minor procedures inside the joint such as cortisone injections or lavage (flushing) of the joint. It's rare for major surgery ever to be necessary in a case of TMD. Again, it's important to try the wide range of conservative, reversible treatments available, and give them enough time to work as they almost always prove effective. The first step is an examination at the dental office. To learn more about available treatment options, view this Chart on TMD Therapy
Jaw/TMJ
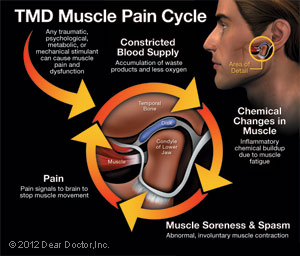
If you experience ongoing pain in the area near your ear, your jaw or the muscles on the side of your face, possibly accompanied by a clicking or popping sound or restricted jaw movement, you may be suffering from TMD — an abbreviation for Temporomandibular disorders. Sometimes people incorrectly use the term TMJ to refer to these problems, when in fact TMJ is the abbreviation for the temporomandibular joint — or jaw joint — itself. So while you definitely have a TMJ (two of them in fact), you may or may not have TMD.
TMD, then, describes a group of conditions characterized by pain and dysfunction of the TMJ and/or the muscles surrounding it. It's not always so easy to figure out exactly what's causing these symptoms, but the good news is that most TMD cases resolve themselves with the help of conservative remedies that you can try at home. In fact, it's important to exhaust all such reversible remedies before moving on to anything irreversible, such as bridgework or surgery.
The two TMJs that connect your lower jaw, the mandible, to the temporal bone of the skull on either side, are actually very complex joints that allow movement in three dimensions. The lower jaw and temporal bone fit together as a ball and socket, with a cushioning disk in between. Large pairs of muscles in the cheeks and temples move the lower jaw. Any of these parts — the disk, the muscles or the joint itself — can become the source of a TMD problem. If you are in pain, or are having difficulty opening or closing your jaw, a thorough examination can help pinpoint the problem area; then an appropriate remedy can be recommended.

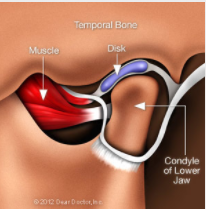
Causes of TMJ
As with any other joint, the TMJ can be subject to orthopedic problems including inflammation, sore muscles, strained tendons and ligaments, and disk problems. TMD is also influenced by genes, gender (women appear to be more prone to it), and age. Physical and psychological stress can also be a factor. In some cases, jaw pain may be related to a more widespread, pain-inducing medical condition such as fibromyalgia (“fibro” – connective tissues; “myo” – muscle; “algia” – pain).
Signs and Symptoms of TMD
Clicking Sounds — Some people with TMD hear a clicking, popping or grating sound coming from the TMJ when opening or closing the mouth. This is usually caused by a shifting of the disk inside the joint. Someone standing next to you might even be able to hear it. Clicking by itself is actually not a significant symptom because one third of all people have jaw joints that click, studies show. However, if the clicking is accompanied by pain or limited jaw function — the jaw getting “stuck” in an open or closed position, for example — this would indicate TMD.
Muscle Pain — This can be felt in the cheeks (masseter muscles) and temples (temporalis muscles), where the two big pairs of jaw-closing muscles are located. If you feel soreness and stiffness upon waking up in the morning, it's often related to habits such as clenching and/or grinding the teeth at night. If you have this type of nocturnal habit, a custom-made nightguard should be very helpful in decreasing the force applied to your teeth, which will in turn allow your muscles to relax and relieve pressure on your jaw joints. Other self-care remedies are discussed below (please see Relieving the Pain).
Joint Pain — Pain that's actually coming from one or both jaw joints technically would be described as arthritis (“arth” – joint; “itis” – inflammation) of the TMJ. Radiographs (x-ray pictures) show that some people have arthritic-looking TMJs but no symptoms of pain or dysfunction; others have significant symptoms of pain and dysfunction but their joints look normal on radiographs. There is no cure for arthritis anywhere in the body, but medication can sometimes help relieve arthritic symptoms.
Relieving the Pain
Once you have been examined, a strategy for treating your condition and managing your pain can be developed. Sometimes a temporary change to a softer diet can reduce stress on the muscles and joints. Ice and/or moist heat can help relieve soreness and inflammation. Muscles in spasm can also be helped with gentle stretching exercises. Non-steroidal anti-inflammatory medications and muscle relaxants can also provide relief.
Other Treatment Options
Severe TMD cases may require more complex forms of treatment, which might include orthodontics, dental restorations like bridgework, or minor procedures inside the joint such as cortisone injections or lavage (flushing) of the joint. It's rare for major surgery ever to be necessary in a case of TMD. Again, it's important to try the wide range of conservative, reversible treatments available, and give them enough time to work as they almost always prove effective. The first step is an examination at the dental office. To learn more about available treatment options, view this Chart on TMD Therapy